Dr Manish Bothale explains the advantages of continuous glucose monitoring system.
Ms Y is 22 years old with Type 1 Diabetes since age 14. She is a student at a business school. Recently her schedule has become busier due to her rigorous studies and business travelling. She often suffers from repeated episodes of hypoglycaemia (low blood glucose). She has never faced this challenge and has become hesitant to administer adequate insulin doses in fear of low blood glucose levels. This has led to higher blood glucose levels and an increased risk of long-term complications associated with Diabetes such as damage to eyes and kidneys. She is becoming increasingly frustrated with her Diabetes management and is unsure of what to do next.
Not so uncommon
Unfortunately, this is a common situation. The management of Diabetes can easily be disrupted as changes in everyday life have a profound impact on blood glucose control. Even small changes in people’s lives such as forgetting to eat or increased activity throughout the day can have a major impact on blood glucose levels. Often these changes are unrecognised by the patient leaving them confused as to why their glucose levels have drastically changed.
Recent advances in Diabetes technology such as the continuous glucose monitor (CGM) are aimed at helping people with Diabetes better track their glucose levels and adjust their insulin regimen quickly and easily. This technology is extremely valuable, especially in India, where Diabetes is one of the biggest health issues facing the country.
Diabetes, particularly, Type 1 Diabetes is difficult to manage. Optimal blood glucose control is essential in reducing long-term complications of Diabetes such as eye and kidney damage and foot infections leading to amputations. It is estimated that decreasing haemoglobin A1c (HbA1c) levels (the measurement used to assess average blood glucose levels over a
three-month period) by 1 per cent can reduce the risk of Diabetes-related deaths by 21 per cent, eye, kidney and foot complications by 37 per cent and heart attack by 14 per cent. Therefore, American Diabetes Association (ADA) and other Diabetes organizations recommend having a target HbA1c level of less than 7 per cent without increasing the risk for low blood glucose. Achieving this target HbA1c is not easy for most patients with Diabetes especially those who are on insulin therapy as there is a risk of low blood glucose with aggressive insulin therapy. However, the newer technologies such as insulin pump and continuous glucose monitoring system helps people with Diabetes achieve their target glucose control without substantial high and low blood glucose levels fluctuation. Here in this article, we will talk more about continuous glucose monitoring system (CGM).

New technology to the rescue
Self-monitoring of blood glucose (SMBG) refers to blood glucose testing at home by people who have Diabetes. Self-monitoring requires willingness on the part of the individual as well as commitment to test blood glucose levels at the designated time every day. Often time it is seen that fear of physical pain or anxiety about sugar levels could lead to avoidance or errors while testing. It also does not present the entire picture as readings only indicate blood glucose levels at the time of testing and not as an average of the entire day.
If we think back to Ms. Y, who is a college- aged woman who had previously managed her Diabetes well until changes in her life threw her off that delicate balance. Now she is hesitant to take adequate insulin in fear of low blood glucose which is leading to a rise in her HbA1c level. Unfortunately, this is commonly seen. One that is often difficult for patients and physicians to reverse.
Luckily, there is a new technology on the horizon in the form of continuous glucose monitoring that shows promising results for helping patients consistently track their blood glucose levels and make adjustments to their medications quickly and effectively. The remainder of this article seeks to explain how CGMs work, how they benefit the physician and patient and what the future holds for this promising technology.
Continuous glucose monitoring explained
Continuous glucose monitor is a small wearable device that measures blood glucose automatically throughout the day and night. It also notifies you of high and
low blood glucose levels so you can take action to keep your blood glucose under control and prevent severe high or low blood glucose levels. A tiny electrode called a glucose sensor is inserted under the skin to measure glucose levels in tissue fluid. It is connected to a transmitter that sends the information via wireless radio frequency to a monitoring and display device. The device can detect and notify you if your glucose is reaching a high or low limit.
History of CGM
CGM system is one of the biggest advancements in Diabetes management in recent years. Until early 1990s, finger stick glucose monitoring by blood glucose meters was the standard way to measure blood glucose and monitor the glycaemic control in people with Diabetes. However, finger-stick glucose measurements are single-point blood glucose estimations and patients have to prick their fingers multiple times a day in order to obtain glucose values at different points of the day. This limitation led to the development of CGMs in the late 1990s. CGM has become a popular tool to monitor blood glucose and manage Diabetes in most developed countries. Currently, it is estimated that 15 per cent of people with Type 1 Diabetes use CGM technology in the United States.
Technology explained
CGMs work by inserting a small sensor, as thin as a strand of hair, under the skin of the abdomen. This sensor monitors glucose levels in tissue fluid (also known as interstitial fluid). Each sensor is made from platinum and coated in bioactive enzymes that help detect blood glucose levels. The enzymes remain active for up to 14 days
(depending on the CGM types) and then the sensor must be replaced. A small transmitter attached to the sensor sends glucose information wirelessly every 5 minutes to a receiver. The receiver then displays the current glucose level and blood glucose trend graphs to the patient. The sensor must be calibrated via traditional finger prick glucometer in order to remain accurate. The longer the patient wears the CGM the more accurate the readings become due to refinement of a copyrighted algorithm specific to the brand of CGM
being used. The sensor and transmitter are waterproof, making it more convenient and reliable for the patient. Also, some CGMs do not require an extra receiver, but instead send all blood glucose information to the patient’s smart phone or smart watch. This eliminates the need for him or her to carry around an extra device specifically for blood glucose readings.
Advantages of CGM in real time
Diabetes is a very difficult disease to manage. It takes a great deal of effort from both the patient and physician to create a plan that will achieve the desired HbA1c goal.
Insulin dosage and other Diabetes medications are based on blood glucose trends throughout the day. It is very difficult for patients to predict their blood glucose levels, especially when they are on insulin therapy.
Many factors such as exercise, stress, food, day to day activities can affect the blood glucose. Therefore, CGM helps people with Diabetes become proactive based on blood glucose trends. For example, CGM alarms the patients when blood glucose is high or low so that patient can take insulin or glucose depending on blood glucose without needing to poke their fingers. In addition, CGM tells the patient if blood glucose is trending high or low (even before your blood glucose gets high or low) so that patient can become proactive and avoid high or low blood glucose.
Not only that, your doctor can download these CGM devices in the office in a less than minute and can provide you information about overall blood glucose controls, glucose variations that helps doctors to decide about changing your insulin dose or time. This may reduce the burden on patients and doctors in managing Diabetes.
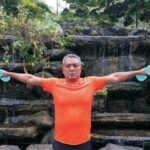
Often athletes who have Diabetes need to keep a closer watch on their blood glucose level fluctuations. A review of pre-exercise and post-exercise sugar level patterns can guide the individual regarding insulin, medication and diet adjustment.
Daily physical and emotional stress can play havoc with sugar control. This impact is often not realised by people with Diabetes. Stress can lead to a sharp increase or decrease in sugar levels.
Especially during illness, CGM devices work as a warning system which can alert the user of extreme sugar level fluctuations and help them avoid both ketoacidosis and severe blood glucose lows.
Current limitations of the CGMs
All current CGM devices measure interstitial glucose (fluid between cells). The delay between systemic glucose level and interstitial fluid glucose is estimated to be between 4 and 26 minutes. This delay limits the accuracy of the CGM, especially when the blood glucose levels are rapidly changing. Most often this results in an overestimation of blood glucose levels. This may cause the person with Diabetes to overdose on insulin, resulting in a rebound low blood glucose level. This is why it is very important for patients wanting to use CGM devices to receive thorough training from an experienced professional.
Unfortunately, these devices are costly and not all patients with Diabetes can afford or use this technology.
What is the future for CGM Use?
The hope is that, as CGM technology advances the costs will further reduce and it will become more accessible to all people with Diabetes. Another hope is that this technology will spawn the development of a “closed-loop (artificial pancreas)”. The artificial pancreas where a patient can wear insulin pump and CGM and insulin pump delivers insulin (basal insulin) automatically based on CGM glucose values and trends by means of intelligently engineered algorithms. That means, patients using artificial pancreas need not to worry about managing Diabetes and keeping the blood glucose in the normal range. However, these systems are not perfect and many researchers are working on improving the artificial pancreas technology for safe use by the people with Diabetes.
To conclude
There is a need for people with Diabetes to ensure better control over their sugar levels. Research studies have indicated that CGM can help keep a better check on blood glucose fluctuations, lower HbA1c levels and incidences and degree of low blood glucose levels.
Real time sugar readings allow a person with Diabetes to take immediate action thereby preventing dangerous high and lows. Patterns of sugar fluctuations can be identified and managed with medication or insulin or dietary changes. This can help people with Diabetes maintain a healthy quality of life.