Importance of pancreas
Pancreas plays an important role in digestion of food. It is situated near the stomach close to the liver and small intestine. Pancreas is made up of the exocrine and the endocrine pancreas. The exocrine pancreas produces enzymes and digestive juices that are required to digest the food. The endocrine pancreas produces
important hormones that help maintain glucose levels in the body. The pancreas contains clusters of cells called the islets of Langerhans, which secrete hormones into the bloodstream. The key hormones include:
Insulin: lowers blood glucose levels by facilitating the uptake of glucose into cells.
Glucagon: raises blood glucose levels by signalling the liver to release stored glucose.
Somatostatin: regulates the secretion of other hormones.
Pancreatic health is essential for the proper functioning of other organs. Poor pancreatic function can lead to conditions like pancreatitis (inflammation in the pancreas), Type 1 and Type 2 Diabetes, cystic tumours of the pancreas and pancreatic cancer. One possible reason of pancreatic malfunction is accumulation of excess fat in the body. This affects the liver, muscles and causes insulin resistance. Due to insulin resistance, the insulin produced by the pancreas loses its ability to work efficiently. This causes the pancreas to overwork and produce more insulin.
Ultimately more and more insulin cannot be formed and this results in Diabetes.
Poor functioning
Poor or no pancreatic functioning can cause Type 1 Diabetes, Type 2 Diabetes, acute and chronic pancreatitis and enlarged pancreas. Acute pancreatitis is caused by
 n
n
scarring of the pancreatic tissue which causes inflammation (swelling). When this swelling goes unchecked, it leads to chronic pancreatitis. This in turn results in permanently damaging the pancreas.
Chronic pancreatitis is also known to cause benign and cancer tumours in the pancreas.
Causes of pancreatitis are:
e gallstones e alcoholism e heredity
e high fat and calcium levels
e use of certain medications like antidepressants, immunosuppressant, antibiotics and corticosteroids
Oral medication is required to increase pancreatic functioning.
 n
n
Glucose levels and pancreas
Managing sugar levels is important to keep the pancreas healthy. If the sugar levels rise beyond a certain point, they start to have an adverse effect on the pancreas called glucotoxicity. Glucotoxicity causes the beta cells of the pancreas to be destroyed due to continuous high blood glucose levels (chronic hyperglycaemia). It can also result in worsening of Diabetes and the start of Diabetes-related complications.
Type 1 Diabetes and pancreas
Type 1 Diabetes affects the endocrine pancreas. In Type 1 Diabetes, the beta cells are destroyed by the immune system affecting insulin production in the body.
This causes high sugar levels in the blood. Type 1 Diabetes also affects the exocrine pancreas. Type 1 Diabetes causes the exocrine pancreas to shrink by 50 per centof its original size. Pancreatic functioning also decreases.
Type 2 Diabetes and pancreas
People with Type2 Diabetes are more a trisk of developing pancreatitis. Studies have also shown that there can be a lot of scarring in the pancreas in Type2 Diabetes. We believe that high glucose levels and other reasons causes carring in the pancreas
 n
n n
n
Artificial pancreas
An artificial pancreas, also known as a closed-loop system or automated insulin delivery (AID) system, is a technology designed to automate blood glucose management in people with Diabetes, particularly Type 1 Diabetes. It mimics the glucose- regulating function of a healthy pancreas by continuously monitoring blood glucose levels and automatically administering the appropriate amount of insulin.
How does it work?
An Automated Insulin Delivery Systems (AID) system typically comprises three main components:
e Continuous Glucose Monitor (CGM): A sensor that measures glucose levels in the interstitial fluid throughout the day and night.
 n
n
e Insulin Pump: A device that delivers insulin through a catheter placed under the skin.
e Algorithm/Control System: Software that interprets glucose data from the CGM and adjusts insulin delivery from the pump accordingly.
The system works in a closed-loop manner, where glucose readings are sent to the control algorithm, which then calculates the required insulin dose and signals the pump to administer it.
The artificial pancreas does not, in fact, actually aim to replace the entire biological organ, just its beta cells. In Type 1 Diabetes, the pancreatic beta cells – the only cells in the body able to produce insulin – are destroyed by a malfunctioning immune system. The beta cells in people with Type 2 have also stopped producing an adequate insulin supply. Insulin’s job is to move glucose from the blood into the body’s cells, where it can be used for energy. A shortage of insulin traps glucose in the blood, leading to the damaging high blood glucose levels that characterise Diabetes.
People with Type 1 Diabetes, who would benefit the most from an artificial pancreas and some with Type 2, need to inject or pump insulin into their bodies to survive. Figuring out just how much insulin is appropriate can be difficult. Research shows that near – normal blood glucose levels can help stave off devastating Diabetes complications that ravage the eyes, nerves, kidneys and heart. However, maintaining that tight level of control requires insulin doses that walk the line between enough and too much. To make matters worse, the body’s response to insulin can vary widely and unpredictably, depending on factors like food, exercise, stress and illness. This volatility can leave a person with excess insulin in the body, which may cause severe hypoglycaemia (low blood glucose). The danger is particularly grave, and lows are most common, during sleep.
While the artificial pancreas is not a cure for Diabetes, it could help people get all the complication -averting benefits of tight control without the serious dangers of hypoglycaemia.
 n
n
Availability of AID systems
Several companies and research institutions are developing AID systems. Notable developers include:
-
Medtronic
-
Tandem Diabetes Care
-
Insulet Corporation
-
Beta Bionics
-
Bigfoot Biomedical
The US Food and Drug Administration (FDA) has approved several AID systems, including:
e Medtronic MiniMed 670G/780G e Tandem Control-IQ Technology e Omnipod 5 (Insulet Corporation)
As of the latest, Medtronic’s MiniMed 780G and some offerings from Ypsomed are available in India. The cost of a closed-loop system can vary widely based on the components and region. In India, the cost of an AID pump can range from 6.5 to 8 lacs rupees. AID system users will also require to spend approx. 20-25 k on consumables and sensors/month.
Do-It-Yourself (DIY) AID system
Yes, it is possible to create a DIY AID system. The most well-known DIY system is Open APS (Open Artificial Pancreas System), which uses open-source software and commercially available hardware.
However, DIY systems carry risks, as they are not regulated by health authorities, and users need significant technical expertise to implement and manage them safely.
Side effects of artificial pancreas
Potential side effects of using an artificial pancreas include:
Hypoglycaemia: Risk of low blood glucose levels, although AID systems are designed to minimize this risk.
Hyperglycaemia: Risk of high blood glucose levels if the system malfunctions or is not calibrated correctly.
Skin Irritation/Infections: At the site of sensor or catheter insertion.
Technical Issues: Device malfunctions or connectivity issues.
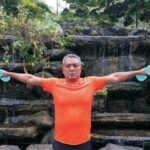
AID system and diet and fitness
Using an AID system can provide more flexibility in diet and exercise routines, as the system continuously adjusts insulin delivery based on real-time glucose levels. However, users still need to manage carbohydrate intake and monitor their physical activity to optimize system performance.
Future of AID systems
The future of AID systems looks promising with ongoing advancements in technology and algorithms. Future developments may include:
Improved Algorithms: More sophisticated algorithms that can predict glucose trends and adapt to various physiological conditions.
Integration with Other Wearables: Enhanced data collection from multiple sources to provide more accurate glucose management.
Bi-Hormonal Systems: Systems that deliver both insulin and glucagon to better mimic natural pancreatic functions.
Increased Accessibility: Wider availability and affordability through improved manufacturing processes and insurance coverage.