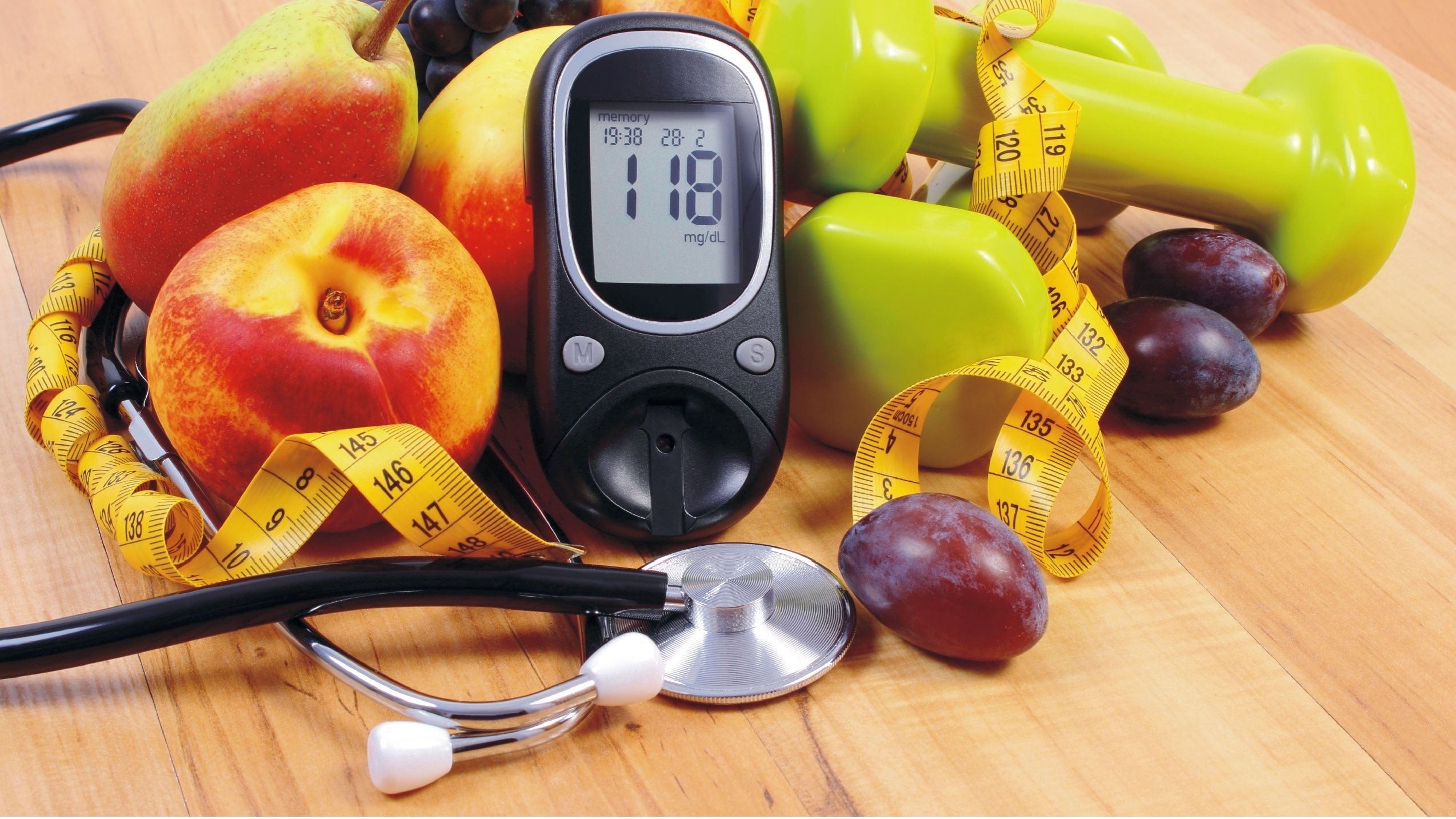
I have Type 2 Diabetes for 6-7 years and was initiated on insulin therapy six months ago. Is it possible to stop insulin and just manage my condition with diet and exercise or will I be taking insulin life-long?
Generally, people with Type 1 Diabetes require insulin for survival but that is not the case in your scenario since you have Type 2 Diabetes. The common indications to start insulin in people with Type 2 Diabetes are:
Failure to achieve the desired glycaemic control with diet, exercise and medications.
To achieve rapid glucose control in case of severe hyperglycaemia (raised blood sugar) due to a stressful event (For eample: dental procedure or hospitalisation for a chest infection). In such cases, insulin is stopped once the acute stress is relieved.
When the HbA1c (average sugar for last three months), at the time of diagnosis is 9 per cent or if the person has severe symptoms like marked weight loss or excessive thirst, urination or hunger.
When oral medications could not be administered due to an associated medical illness such as kidney failure or liver failure. However, as the condition improves your doctor may discontinue insulin.
Once you acquire good glycaemic control, your doctor may advise oral medications along with proper diet and exercise. Keep in mind that insulin can help you achieve your blood glucose target, which will make you feel better and have more energy. With the advances in insulin administration devices with thinner needles, injecting insulin has become more comfortable and less painful.
Dr Ashutosh Pakale
Consultant Physician
 n
n
Regular exercise is extremely important to control Diabetes. But is there a point at which the exercise is so intense that it actually becomes dangerous?
Yes, excessive exercise is dangerous. Exercise must be managed correctly. The risk can be minimised or completely avoided by seeking guidance from doctors. Your doctors and you working together can construct a plan to manage Diabetes before, during and after the activity.
Heavy exercise can increase blood glucose levels and also increase the risk of hypoglycaemia in people with Diabetes on insulin treatment. People with few diabetic complications such as retinopathy (eye damage), neuropathy (nerve damage) may have untoward effects if vigorous activities are done. Exercise that’s too hard can raise your blood sugar by making it harder for your muscle cells to use insulin. Regular, moderate level of exercise is healthy and safe for people with glaucoma but extreme exercise that pushes and strains your body can raise pressure inside the eye. This pressure is known as intraocular pressure that is high IOP can lead to optic nerve damage and vision loss.
Exercise also improves your nerve function and promotes nerve cell regeneration but if you have nerve damage in your feet, avoid repetitive weight bearing exercises such as jogging, prolonged walking and step aerobics. Repetitive stress on the feet that are affected with neuropathy can lead to ulcers, fractures and joint problems.
Choose the exercise that do not put stress on your feet, a constant state of overtraining however can lead to very serious condition called central nervous system fatigue. This could be identified as a feeling of numbness, pain, tingling or burning in the extremities. Blood glucose levels also may rise if you do short bursts of hard aerobic exercise known as high intensity interval training.
It’s okay to exercise. Be aware that blood sugar may rise if you do strength training or high intensity interval training. Consult your doctor, physiotherapist and dietician to avoid any complications before starting or modifying a exercise regime.
Dr Uma Hire (P.T.)
Consultant Physiotherapist
 n
n