Dr Savita Bhat explains the causes and management of diabetic retinopathy.
Many people with Diabetes are often unawarethat Diabetes affcets their vision and causes diabetic retinopathy. Diabetic retinopathy (DR) is an important cause of visual impairment and blindness in people with Diabetes especially amongst those who fall within the working age group. Thus, the morbidity and treatment costs of diabetic retinopathy results in significant economic burden to individuals and society as a whole.
Blindness and visual impairment related to Diabetic retinopathy also has significant impact on the quality of life of people with Diabetes. One in three people will prediabetes will have retinopathy.
What is Diabetic Retinopathy?
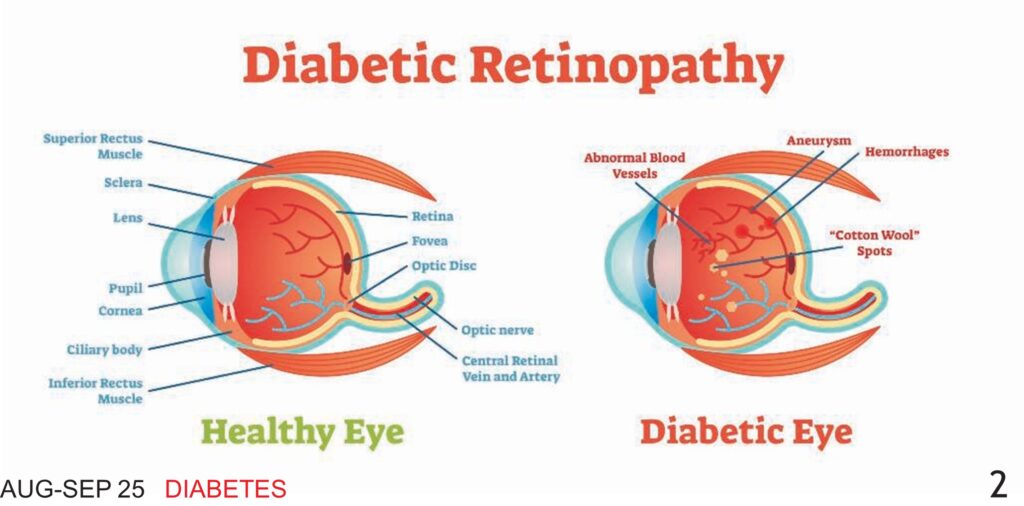
Diabetic Retinopathy is a complication associated with Diabetes affecting small blood vessels of the retina. The retina is a light-sensitive layer which forms the inner lining at the back of the eye. The optics of the eye creates an image of what is seen center of the retina. This functions like the film in a single-lens reflex camera. The image viewed is focused upon the center of the retina called the macula. However, the entire inner lining other than the center also receives and processes light signal and aids in the field of vision.
People at a higher risk of developing Diabetic Retinopathy are those who:
- have Type 2 Diabetes for more than 5-10 years
- have Type 1 Diabetes
- have poor blood glucose control
- have high blood pressure
- have lipid abnormalities
- have anaemia
- smoke
- are pregnant
How is vision affected by Diabetic Retinopathy?
Diabetes can affect various parts of the eye. Common causes are blurry vision due to increased blood glucose, cataract formation, glaucoma, dry eyes, lid cindines and the foremost damaging the retina is diabetic retinopathy.
People with Diabetes are more likely to develop cataracts at a younger age especially if Diabetes is uncontrolled. They are twice as likely to develop glaucoma, but Diabetes’ effect on the retina is the main threat to vision called diabetic retinopathy, this effect of Diabetes on the eyes is the most common cause of blindness in people of 20- 65 years.
Over time, Diabetes causes changes in the tiny blood vessels that nourish the retina. In the early stages, known as non-proliferative or background retinopathy, the small arteries in the retina weaken and begin to leak, forming small, dot-like hemorrhages (blood flow from the ruptured blood vessel) on the surface. These leaking vessels often lead to swelling (edema) in the retina and decreased vision. At this stage, vision may be normal or it may have started to blur or change. About one in four people with Type 2 Diabetes experience this problem. This can happen in the center or multiple areas of the retina
When retinopathy advances, the decreased circulation of the blood vessels deprives areas of the retina of oxygen. Blood vessels become blocked or closed, and parts of the retina die. New, abnormal, blood vessels grow to replace the old ones. They grow along the retina and along the surface of the vitreous or into it (the transparent gel that fills the inner portion of the eyeball).
Unfortunately, these delicate vessels are fragile, incompetent, abnormal and rupture easily. Blood may leak into the retina and vitreous, causing “floaters” (spots that appear to drift in front of the eyes), along with decreased vision. This is called proliferative retinopathy. One in three people with diabetic retinopathy may have proliferative retinopathy. It can lead to severe visual loss or blindness. In the later phases of the disease, continued abnormal vessel growth and scar tissue may cause retinal detachment and glaucoma.
The effect of retinopathy on vision in people with Diabetes varies widely, depending on the stage of the disease. Common symptoms can include blurred vision (often linked to blood glucose levels), early spots in the area, red ringed fields, abnormal colour vision and eye floaters. However, Diabetes may cause other eye symptoms.
Fluid can leak into the center of the macula, the part of the eye where clear, detailed vision occurs. The fluid swells the macula and blurs the vision called macular edema, it can occur at any stage of retinopathy although it is more likely to occur as the disease progresses.
Screening for Diabetic Retinopathy
|
Diabetes is classified broadly into Type 1 and type 2 Diabetes. Any individual with Type 1 or Type 2 Diabetes should be screened retinopathy. The interval for follow up assessments should be tailored to the severity of the retinopathy. In those with no or minimal retinopathy, the recommended interval is four to six months. All individuals with Type 2 Diabetes should be screened at the time of diagnosis. Women with Type 1 or Type 2 Diabetes or women who hope to become pregnant should be screened before conception, during the first trimester, as needed during pregnancy and within the first-year post-partum. All people with Diabetes – both Type 1 and Type 2 – are at risk for diabetic retinopathy.
A trained Ophthalmologist can screen for Diabetic Retinopathy either using Fundus photography or by a dilated fundus examination using indirect ophthalmoscopy. There are several reliable cameras to photograph the stages of retinopathy. Serial photography helps comparison to check progression of the disease. Even in remote rural areas, patients can be screened using portable indigenous cameras.
The physician should be the first point of contact for people with Diabetes. 90 per cent of Diabetic Retinopathy cases (early stages) only require management (hypertension control and lipid level regulation) under the guidance of Physician. Most of patients with diabetic retinopathy need only follow up. Only some need referral to an Ophthalmologist. Hence visual acuity examination and fundus imaging (portable fundus camera) should be a part of the examination protocol at the physician’s clinic.
Management of Diabetic Retinopathy
No treatment is needed for nonproliferative retinopathy, unless there is selling in the inner part of the retina called macular oedema. Important modifiable risk factors include glycaemic (blood glucose) control, blood pressure, anaemia, renal parameters, serum lipid level control. Regular physical activity and cessation of smoking does have a positive influence in preventing progression of Diabetic Retinopathy Regular physical activity in the form of brisk walking, yoga can have a beneficial effect in arresting the progression of Diabetic Retinopathy.
However, one with more advanced forms of Diabetic Retinopathy (which has resulted in bleeding in the eye) should be cautious in performing vigorous exercises requiring heavy breathing or lifting heavy weights which can increase pressure on the tiny fragile new blood vessels causing significant vitreous bleeding and resulting in impaired vision.
Medical management of Diabetic Retinopathy
Laser photo-coagulation is the gold standard therapy in the management of diabetic macular edema and proliferative (severe) form of Diabetic Retinopathy. Laser therapy helps to shrink the abnormal blood vessels, and/or vitrectomy. Treatment works better before the fragile, new blood vessels start to bleed, but even if bleeding has started, treatment may still be possible, depending on the amount of bleeding.
Vitrectomy is done if the bleeding does not resolve within the stipulated time. Blood is removed from the center of the eye and replaced with oil/gas. The surgeon may also remove strands of vitreous attached to the retina that create traction and could lead to retinal detachment or tears in the retina.
This requires more surgery.
Other important options of management include Anti VEGF injections into the vitreous cavity for the management of diabetic macular oedema and proliferate diabetic retinopathy. These injections have largely reduced the need of rigorous management. These pharmacological advances create a significant impact with regards to visual gain in people with diabetic macular oedema.
Surgical Management of Diabetic Retinopathy
Advances in surgical techniques/ visualization systems have changed the scenario of surgical management of diabetic retinopathy. The current common indications for surgical management include non-clearing vitreous bleeding, tractional or combined retinal detachment involving macular area.
To conclude, good metabolic control including A-B-C (A1c- Blood pressure- Cholesterol) along with annual diabetic retinopathy screening by fundus examination is essential for preventing blindness and visual impairment caused due to Diabetic Retinopathy.