What is Periodontitis?
Periodontitis is a chronic inflammatory disease which causes destruction of the supporting structure of teeth i.e. periodontal ligament and alveolar bone. It’s a slowly progressing disease but the tissue destruction that occurs is largely irreversible. In early stages it is usually asymptomatic and not painful. The individual only becomes aware of it when it progresses to tooth mobility. If you improve and maintain good dental hygiene it is fairly preventable.
Periodontal disease and heart health
Studies have shown that bacteria found in periodontal disease including streptococcus sanguis plays a role in strokes and affects heart health. Both go hand in hand. To put it simply, the more bacteria you have in your body the increased likelihood of your heart getting affected. If we reduce long term bacteria, we lower the risk factor to heart disease.
Periodontitis and pulmonary disease
Gum diseases are known to worsen the chronic inflammation in lung diseases such as asthma and COPD. Infected and inflamed gums send distress signal that places rest of the body on alert. This leads to inflammation of lungs. Many inhaled anti-inflammatory broncho-dialators cause dry mouth. This further leads to cavities and gum diseases. Chewing sugarless gum or candy can help you produce more saliva along with an increase in water intake (at least 3 litres a day) which will help in reducing the dry mouth.
Periodontal health and renal dysfunction
Patients with renal dysfunction and on dialysis have been found to have higher prevalence of periodontitis. It is likely the decreased bone mineral density in such patients would increase risk for progressive alveolar bone loss from subsequent periodontal infections similar to what occurs in patients of osteoporosis.
Periodontitis and role of psychosocial factors
Recent studies have shown that psycho- emotional stress may contribute to development of periodontal pathology. Stress activates central nervous system and resultant release of cortisol may cause depression in the immune response. This provides periodontal bacteria an opportunity to proliferate and possibly invade the tissues, eventually causing more extensive inflammatory
response.
Periodontitis and Diabetes
Periodontitis is stated to be the sixth complication of Diabetes. There is a clear relationship between degree of hyperglycaemia (high blood glucose level) and severity of periodontitis. The risk of periodontitis is increased approximately threefold in people with Diabetes as compared to non-diabetics.
The studies have shown two-way relationship between Diabetes and Periodontitis – not only does Diabetes or poor glycaemic control increases risk for periodontitis but also periodontitis has negative effect on glycaemic control.
Both Type1 and Type 2 Diabetes mellitus are associated with elevated inflammatory markers, whereby cytokines play a central role in the host’s response to periodontal biofilm. (Cytokines are small soluble proteins that confer instructions and mediate communication among immune and non-immune cells. A biofilm is the collection of microscopic living things that grow together within a substance that they produce. When not removed regularly, these bacteria cause problems such as periodontal disease, gingivitis, and cavities.) It explains immune-biological connection between Diabetes and periodontal diseases.
Periodontal infection can contribute to the low grade general inflammation associated with Diabetes thus aggravating insulin resistance and glycaemic control in people with Diabetes.
 n
n
Treatment of periodontitis
The treatment of periodontitis is associated with significant reduction in HbA1C levels (i.e. approximately by 0.4 per cent)
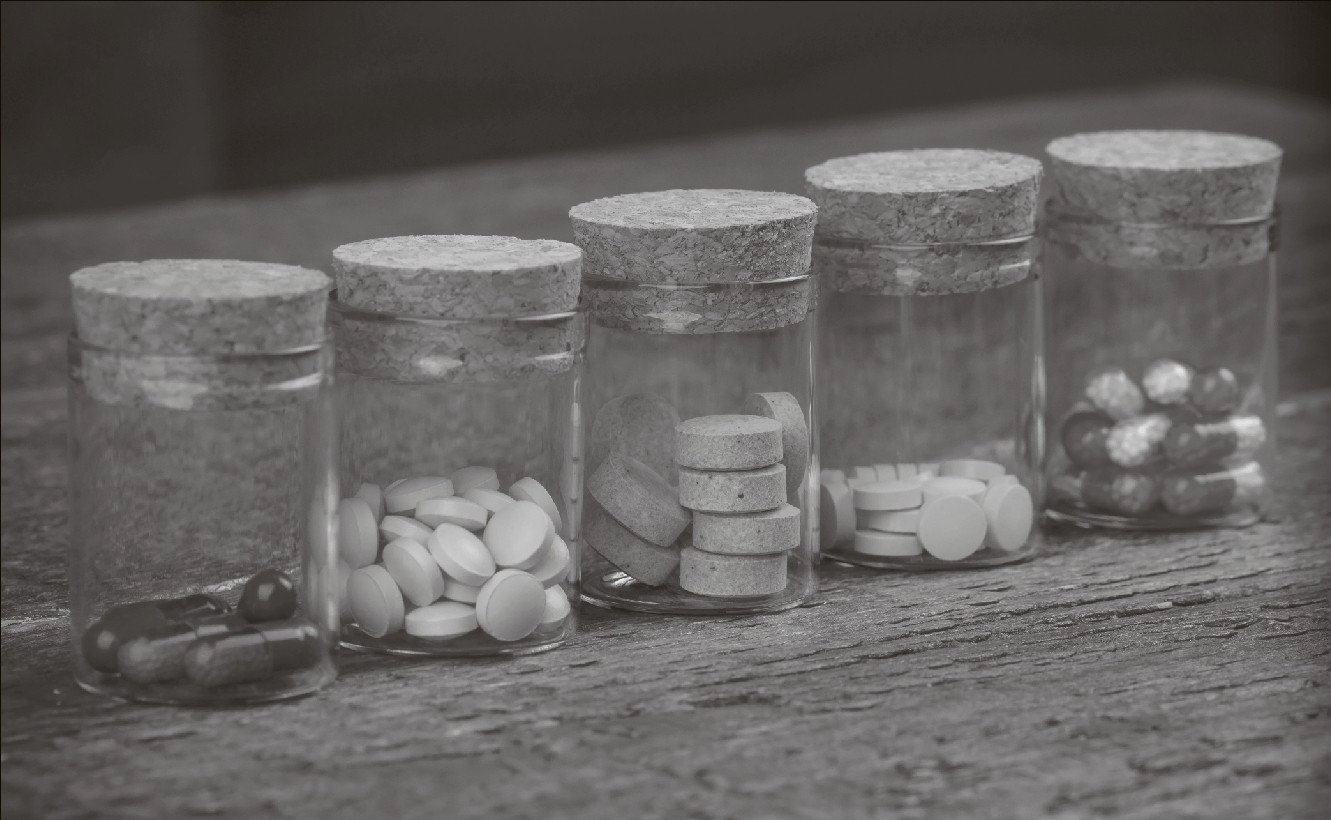
The treatment includes:
1. Non-surgical treatments
e Scaling – Removes tartar, calculus, bacteria from your tooth surface and beneath your gums using ultrasonic device.
e Root planning- Root planning smoothens root surface discouraging build-up of tartar and bacteria contributing to healing and reattachment of the gums to tooth surface.
2. Surgical treatments
Flap surgery (cleaning the roots of the tooth and repairing bone damage)
Soft tissue grafts
Bone grafts
3. Lifestyle changes
Brush twice daily using an electric toothbrush for effective cleaning and plaque removal.
Rinse after every meal or snack.
Floss daily.
Use interdental brush or a water flosser recommended by your dentist
Don’t smoke or chew tobacco.
Take regular dental appointments for professional teeth cleaning.
Dr Nikita Y. Desai, BDS, is Consulting Dentist.
 n
n