Dr Savita Bhat explains the causes and management of glaucoma
Did you know?
- Glaucoma if detected early and treated, will not lead to blindness.
- Cataract and glaucoma are two different diseases. They may be present alone or may coexist in one or both eyes of the patient.
- Glaucoma can be controlled but not
- Glaucoma does not always culminate in blindness.
- Advanced, untreated cataract does not always result in glaucoma.
- Glaucoma treatment surgery is aimed at reducing intraocular pressure and preserving vision.
- An annual eye examination with eye pressure evaluation should be done after the age of forty years, particularly in patients with risk factors.
More about glaucoma
Glaucoma is a leading cause of irreversible vision loss and may lead to blindness if it remains undetected. It may occur in any age group and should be screened in all above ages above 40 years. There are no symptoms in glaucoma and it often remains hidden until later stages impact sight. Therefore, it is often called the silent thief of vision.
Early diagnosis, appropriate treatment and control of eye pressure can preserve vision throughout life. Early detection and treatment of glaucoma can help you to have normal vision throughout life. We have three faculties of vision:
- Visual acuity which is tested with charts
- Colour vision ability to identify hues and colours
- Peripheral vision which is tested with perimetry in glaucoma, stroke and thyroid and pituitary disease. This is usually taken for granted.
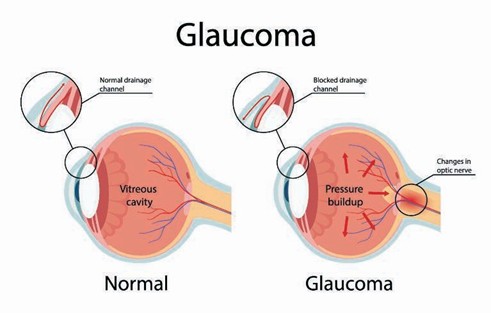
What is glaucoma?
Glaucoma is a group of progressive eye diseases that occurs due to raised eye pressure which damages the optic nerve. The optic nerve is a bundle of fibres which collectively carries visual signals from the eye to the brain. Damage to the optic nerve results in slow progressive loss of side or peripheral vision. It is caused by increased eye pressure (intraocular pressure).
If left untreated, the increased eye pressure causes slow, irreversible damage to the eye’s optic nerve and retinal nerve fibres leading to progressive permanent loss of peripheral vision initially and the not-seeing areas extends to the centre gradually.
The eye functions like a camera; it receives images of the objects and relays messages to the brain through the optic nerve.
This optic nerve has more than two million nerve fibres very similar to the electrical cable containing many fine copper wires. When the pressure inside the eye rises beyond the normal range, optic nerve fibres get damaged progressively.
What causes glaucoma?
Most of us are aware of high blood pressure in the body which can be harmful to health if left untreated. For an analogy just like untreated blood pressure can harm the kidney or lead to cerebrovascular accidents stroke / paralysis. Similarly untreated eye pressure can impact the optic nerve and cause loss of peripheral vision.
The normal eye pressure is 10-21 mmHg with an average of 16 mmHg.
The normal eye pressure is due to the circulating clear fluid called aqueous fluid/aqueous humour (this liquid is not part of the tears on the outer surface of the eye). This circulates in the front of the eye. There is a continuous formation and outflow of this fluid inside the eye.
The fluid forms at the ciliary body behind the iris in front of the lens and drains at the angle in front of the iris between the cornea and the iris – angle of the eye called drainage angle.
The continuous formation and exit of the fluid help maintain the normal health and function of the eye tissue. The eye pressure varies with individual, race and time of the day. The eye pressure like blood sugar and blood pressure is a continuous variable and is subject to change.
Any disturbance in this equilibrium hampers the eye pressure. As the eye is a closed structure and if the drainage area gets damaged, the excess fluid cannot flow out of the eye. The damage to the drainage area can occur in two ways, either mechanical closure or malfunction of drainage.
The pressure exerted by the accumulated channel fluid which is unable to exit from within the eye increases and impinges on the inner structures pushing against the optic nerve causing damage.
Different types of glaucoma
There are two basic types of glaucoma:
- Open-angle type – drainage angle open but malfunctioning
- Closed angle type – drainage angle is closed mechanically
Open-angle glaucoma:
- Functional drainage angle is insufficient to adequately remove aqueous humour of the eye to maintain optimal eye
- Risk increases with
- Risk increases with the family history of glaucoma
- Early stage with pressures (20 mm of hg) with no symptoms
- With advanced disease, the field loss affects the centre and there are abnormalities in vision.
Closed angle glaucoma:
- The drainage angle is mechanically closed as angle is narrow – hereditary and/or increased lens thickness
- These patients usually have shorter eyeballs and are far-sighted. They have ‘+’ glass power for distance.
People with short eyeball have crowding of structures in the front of the eye and space between the iris and the cornea is further compromised. The iris in such eyes mechanically blocks the drainage area similar to a road traffic block. The aqueous fluid builds up within the eye and it can raise the eye pressure up to 3-4 times (up to 40-60 mmhg) from normal and subsequently cause optic nerve damage.
Pressures and the amount of optic nerve damage may depend on the amount of angle closed. This closed-angle variety of glaucoma may produce many alarming symptoms:
- Eye pain with/or without one-sided headache
- Redness
- Watering
- Nausea/vomiting
- Coloured haloes around light or rainbows
This condition is an eye emergency. Unless detected and treated appropriately it can lead to blindness.
Who are at risk of glaucoma?
- Elderly age group
- Positive family history of glaucoma and age >40 years
- Farsighted (plus power for distance – angle closure) and short-sighted (minus power for distance open angle)
- Past history of eye injuries
- Thinner central corneal thickness
- Certain systemic diseases including Diabetes mellitus, migraine, obstructive sleep apnoea, hypertension, thyroid disease
- Persons on steroid therapy – rheumatoid arthritis, -post-renal transplant, asthmatic, chronic obstructive pulmonary disease
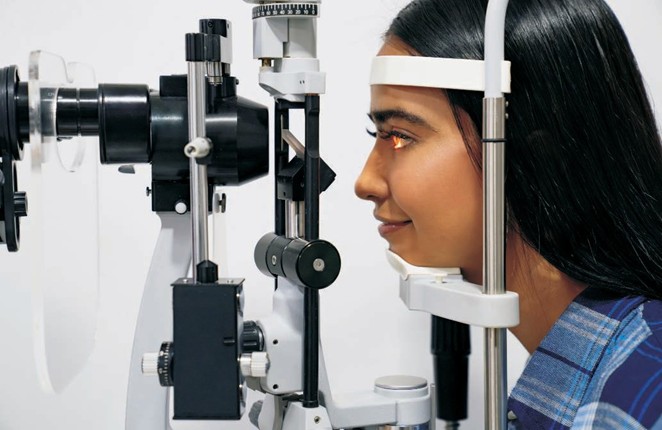
How is glaucoma detected?
A complete routine eye examination helps to detect glaucoma. Patients at risk should undergo appropriate tests as advised along with regular follow up.
What are the tests for glaucoma?
Specific tests for glaucoma are done for measuring
- The pressure of the eye using lipid standard applanation tonometry
- View of the drainage angle using
- gonioscopy or by anterior segment optical coherence tomography (OCT). o Closed angle glaucoma can be
screened by viewing the drainage
angle using a gonioscopy
o Or doing and anterior segment scan to measure the angle on OCT
- Examination of the optic nerve- serial photography on subsequent visit helps detect progression of disease.
- Test to detect the extent of damage to the optic nerve using the peripheral field of vision or extent of side vision ability or the computerized automated
- Optic nerve head photography can be done for documentation of optic nerve head structure and level of damage
- Optical coherence tomography:
- Retinal nerve fibre assessment to detect optic nerve head damage to the nerve tissues with the fluctuating internal eye pressure.
- ganglion cell layer
All the tests may not be needed for all the
patients. Some tests are, however, required at regular intervals-intraocular pressure, gonioscopy and optic nerve end assessment along with perimetry.
Additional tests such as UBM (ultrasound bio- microscopic examination) may locate the extent of the block and give additional information about the structures behind angle.
Treatment
Drops
Damage to the optic nerve is irreversible but progression and further field loss can be prevented with eye drops. The eyedrops reduces aqueous formation or increases drainage thereby reducing eye pressure
Nd:YAG peripheral laser iridotomy
Laser is done for select patients of glaucoma and particularly in the closed/narrow-angle. The Nd:YAG peripheral laser iridotomy is done to relieve the mechanical block at the drainage angle. This makes alternative conduit for circulation of aqueous fluid relieving fluid build-up. For example – during a vehicular traffic block, one tends to take a detour to
avoid the traffic block. This Nd:YAG laser iridotomy is like a detour to make an alternate channel for fluid circulation. This is an outpatient procedure and does not require hospitalization.
Surgery
Surgery for glaucoma, unlike popular belief, will not eradicate glaucoma. This may be combined with cataract surgery for better results.
This is done only if:
- Drops fails to keep the eye pressure under control.
- Elderly patients or patients who are non-compliant with
- Despite adequate medical therapy and compliance , the peripheral vision shows progressive worsening over
- Coexisting cataract and glaucoma may need a combined surgery for both cataract and glaucoma or separate surgeries for either.
The most common glaucoma surgery (the gold standard) is trabeculectomy. In this glaucoma surgery, a well -covered or guarded conduit/channel is created for the aqueous to pass out from inside of the eye to its exterior. This surgery relieves or lowers the eye pressure and thereby reduces pressure on the already damaged optic nerve. To keep the surgically created conduit patent special agents like Mitomycin C, Ologen etc. may be used. It is important to note that trabeculectomy:
- Does not reverse the field loss/vision loss in an eye with severe loss.
- It is done to lower the eye pressure
- It can be combined safely with
Shunts
In some advanced glaucoma cases, it is difficult to perform trabeculectomy or in some, there is a higher chance of the trabeculectomy surgery to fail, like neovascular glaucoma or eyes having undergone multiple surgeries/post trauma, such patients are advised shunt/stent surgeries. All patients do not need all treatment modalities. There are no shortcuts to glaucoma management. Long term drops usage and regular follow up are both needed for preserving fields.
All the glaucoma patients cannot be treated with laser, stents and/or surgeries. Some need only drops whereas others may need laser and/or drops and so on.
How long should one use the eyedrops?
Glaucoma is a chronic, slow-progressing disease. The drops need to be
used lifelong unless some other intervention has been done.
Most open-angle glaucoma can be treated and controlled with eye drops. Like other chronic diseases (diabetes and hypertension) this requires long treatment and regular review.
Why does the doctor insist on testing the fields?
Glaucoma is a disease which slowly damages the peripheral vision. A patient coming for glaucoma follow up in the clinic can have only eye pressure measured at that particular time. Eye pressure can vary and cause variable damage to the nerve despite treatment.
Therefore, a peripheral visual field assessment is mandatory for all glaucoma patients at the time of detection and for follow up. Also, if the damage is severe and approaching the centre a closer follow up on peripheral fields is better to alter treatment. If the peripheral fields are stable, regular review is required.
Dr Savita Bhat is Senior Consultant in Glaucoma, Medical Retina and Phaco Surgeon at the Chellaram Diabetes Institute. She has published extensively in the field of Glaucoma, with several publications in leading journals, including the American Journal of Ophthalmology and the Journal of Glaucoma (USA) and Retina. She has won best research paper awards at the national and state levels on five occasions, Including the Best Neuro-ophthalmolgy Research Paper at the national level in January 2000, and the prestigious Siva Reddy Research Award at the state level in the year 2009.